By Judith Elaine Halek
Photos and Article Copyright @ 1987
Judith Elaine Halek
Twelve years ago, if I was to mention waterbirth to someone on the street, or a pregnant couple I was working with, most would not know what I was talking about. Now, in 1997, after two International Waterbirth Conferences, media exposure from two segments of 20-20, 60 Minutes, two programs of the Phil Donahue Show, an accidental water birth in a bathtub mentioned on the Oprah Winfrey Show, a Good Morning America segment, America’s Talking; Alive and Wellness highlight, numerous articles and countless parents choosing this alternative approach to childbirth, water birth has become a household term.
In 1985 you could count on one hand the number of books and video tapes available on the topic. Now, you’ll need your other hand, both feet, a friend’s set of limbs and possibly another set of limbs from the community of people, to count the information available. Bibliographies, medical protocols, world wide web are overflowing with information. As with everything that’s alternative and unfamiliar, it takes time for the studies to be calculated and presented in the medical journals.
The Society of Obstetricans and Gynecologists of Canada is preparing to release what may be the most comprehensive guidelines for the management of normal pregnancy and delivery in North America. The 78 page guidelines, to be distributed to all Canadian physicians practising obstetrics, represent an update of SOGC’s existing antenatal guidelines. 1 The SOGC guidelines endorse waterbirths with instructions for safe practice, which primarily involves lifting the baby’s head out of water as soon as it is born.
Sheila Kitzinger’s “Letter from England: Is Water Birth Dangerous?” in the Birth Journal  22:3 September 1995 is an excellent review of the first International Conference on Waterbirth, Exploring the Issues, which took place in London, April 1-2, 1995. This conference attracted over 1,500 participants from 36 countries and reported on at least 19,000 births. Janet Balakas of the Active Birth Movement, Beverly Lawrence Beech of the Association for Improvements in Maternity Services, Jay Ingrey of Splashdown Waterbirth Services and Sheila Kitzinger organized the conference.
22:3 September 1995 is an excellent review of the first International Conference on Waterbirth, Exploring the Issues, which took place in London, April 1-2, 1995. This conference attracted over 1,500 participants from 36 countries and reported on at least 19,000 births. Janet Balakas of the Active Birth Movement, Beverly Lawrence Beech of the Association for Improvements in Maternity Services, Jay Ingrey of Splashdown Waterbirth Services and Sheila Kitzinger organized the conference.
The second International Conference; First North American Conference on Nurturing Women: Integrating Water into Maternity Care, held in Greensboro, North Carolina on April 12-14, 1996 was organized by Joanne Zaleski with Wake Area Health Education Center, Barbara Harper with Global Maternal/Child Health Association, Inc, (GMCHA), North Carolina’s ACNM, the University of North Carolina School of Medicine, North Carolina Department of Environment, Health and Natural Resources and Maternal Child Health Division. There were 403 participants, and eight countries represented.
There is a projection date for a third International Conference scheduled for Spring of 1997 in the United States and a fourth Conference in 1998 back in London.
Dr. Michael Rosenthal, formerly the obstetrician at the Family Birthing Center in Upland, Southern California reported at both conferences on his 10 years experience and 948 water births. Dr. Rosenthal brought the concept of waterbirth into a medical setting in the United States in 1985. “Only nine percent of women had drugs for pain relief, compared with approximately 80 percent in hospitals with a similar patient population in the area. The cesarean section rate was under 10 percent but 34 percent at the adjacent community hospital and 86 percent of women with previous cesarean sections gave birth vaginally.” 2
Studies presented at the Conferences revealed that fewer babies needed resuscitation, fewer went to the intensive care nursery, fetal heart rates were significantly more likely to be abnormal on land than in water, women needed fewer pain-relieving drugs when in water, and episiotomy rates were reduced from 38 to 19 percent. 3
 Dr. Faith Haddad, a consultant obstetrician at the Hospital of St. John and St. Elizabeth, London, discussed water births that had occurred since 1987. Data gathered in 1993 and 1994 contained vital information confirming that water reduces the use of analgesia, helps to keep perineum’s intact yields healthier babies and can accelerate the second stage of labor. Dr. Haddad stated that 76 percent of the women studied, used water during labor and birth.
Dr. Faith Haddad, a consultant obstetrician at the Hospital of St. John and St. Elizabeth, London, discussed water births that had occurred since 1987. Data gathered in 1993 and 1994 contained vital information confirming that water reduces the use of analgesia, helps to keep perineum’s intact yields healthier babies and can accelerate the second stage of labor. Dr. Haddad stated that 76 percent of the women studied, used water during labor and birth.
Water labor and birth has been known to help lower blood pressure, reduce edema, help reduce asthmatic responses. The water also enables a women to organically discover her birth position.
Paul Johnson, a physiologist and specialist in fetal breathing riveted attention as he spoke at the first Conference about what happens before and immediately after birth. In his research, the main factor involved with the first breath is the chemoreceptors in the larynx. During pregnancy, the lungs, of the fetus, “breathe” off and on (fluid moves through them). About 48 hours before labor, the prostaglandins in the fetus increase and “fetal” breathing stops. The baby continues to receive oxygen only through the placenta until specific chemical changes trigger the breathing after birth.
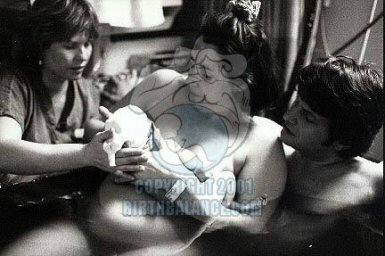
When the baby is born into water, water goes into the larynx, the chemoreceptors are stimulated and this in turn triggers the dive reflex, inhibiting breathing, slowing heart rate, and reducing the need for oxygen. The glottis is closed, swallowing occurs instead of aspiration and the baby continues to receive oxygen from the placenta. In other words when the newborn is born into water, it continues to experience fetal circulation. The baby does not attempt to breathe under water.
As the baby emerges from the water and experiences the change in air pressure, the chemoreceptors in the larynx are stimulated, there is a change in the PH of the cerebrospinal fluid, and the respiratory center in the brain is commands the baby to breathe. The placenta continues to supplies oxygen through the cord for a number of minutes while this transition takes place. Other factors, such as changes in light, sound, temperature and gravity affect the breathing as well.
In all the studies presented at both conferences, there was never a report of fetal or  maternal death or infection due to the water labor or birth. Some medical caregivers believe the water dissipates the bacteria. The key is to make sure the tubs are cleaned with a strong bacterial agent and a chlorine bleach rinse. Bensilkonium spray (diluted 4%) is used after the scrub. Bacterial cultures should be taken monthly and any debris that accumulates while the mother is in the water must be strained out as quickly as possible with a disposable fish net.
maternal death or infection due to the water labor or birth. Some medical caregivers believe the water dissipates the bacteria. The key is to make sure the tubs are cleaned with a strong bacterial agent and a chlorine bleach rinse. Bensilkonium spray (diluted 4%) is used after the scrub. Bacterial cultures should be taken monthly and any debris that accumulates while the mother is in the water must be strained out as quickly as possible with a disposable fish net.
Contraindications for the use of water for labor or birth include anticipated birth complications anticipated, thick meconium in amniotic fluid (as there would be a need for perineal oronasal suctioning,) any obstetrical risk that would be cause for transfer to “high risk” unit, fetal distress, membranes ruptured and the amniotic fluid consistency and color not known, prolonged rupture of membranes (selectively greater than 24 hours with a maternal temp). 4
The use of water is not just another technique. It provides direct phisological benefits to mother and baby by increasing comfort and reducing medical interventions. And babies like it. A father of five who’s last two babies were born under water, swears his waterbabies looked happier and calmer at birth than his “airborn” babies.
FOOTNOTES
1. Medical Post, Vol 32 (5), 1996, page 1. “Healthy Beginnings…Guidelines for care during pregnancy and childbirth.”
2. Birth Journal 22:3 September 1995, Sheila Kitzinger’s Letter from England: Is Water Birth Dangerous?
3. Analysis of first 501 water births a t hospital in Bensburg, Germany. First International WaterBirth Conference, London, April 1-3, 1995.
4. Prodedures and Protocols for Hydrotherapy for Labor and Birth for use @ Harris Regional Hospital, Sylva, NC, July 1995.


 1. October 2, 1993 at 12:22 a.m., an 8 pound 14 ounce beautiful baby girl, Ariella Renee Garmaise-Schlossberg, her parents Judy and Boris, medical caregiver, Dr. Juanita Jenyons marked the first successful water birth at Roosevelt Hospital.
1. October 2, 1993 at 12:22 a.m., an 8 pound 14 ounce beautiful baby girl, Ariella Renee Garmaise-Schlossberg, her parents Judy and Boris, medical caregiver, Dr. Juanita Jenyons marked the first successful water birth at Roosevelt Hospital. history presented itself in the first United States, documented hospital frank breech underwater birth. The courageous parents of newborn, Damon, are Stacie Teele and Dan Varrichione. Dr. Gae Rodkey was the medical caregiver.
history presented itself in the first United States, documented hospital frank breech underwater birth. The courageous parents of newborn, Damon, are Stacie Teele and Dan Varrichione. Dr. Gae Rodkey was the medical caregiver. 4. Come July 7, 1994, Janis Enzenbacher MD, chose water as a labor and birth tool for the underwater birthing of her daughter Eva Liana, entering the world at 11:11 pm with Dr. Rodkey as the attending physician and Isadora Guggenheim as the attending Labor Support Doula and Massage Therapist.
4. Come July 7, 1994, Janis Enzenbacher MD, chose water as a labor and birth tool for the underwater birthing of her daughter Eva Liana, entering the world at 11:11 pm with Dr. Rodkey as the attending physician and Isadora Guggenheim as the attending Labor Support Doula and Massage Therapist. ward in Roosevelt Hospital. The OB ward no longer allows parents to bring in their portable tubs. The birth center has 3 rooms with 3 tubs to labor, but not to birth in. It is my hope that eventually the birth center will open its doors to the water birth option as well.
ward in Roosevelt Hospital. The OB ward no longer allows parents to bring in their portable tubs. The birth center has 3 rooms with 3 tubs to labor, but not to birth in. It is my hope that eventually the birth center will open its doors to the water birth option as well.
 been an advocate of midwifery for the past 12 years. After researching international statistical outcomes regarding midwifery vs. obstetrical care, midwives have far exceeded the lower infant mortality rates, fewer medical interventions and higher results in more empowering births.
been an advocate of midwifery for the past 12 years. After researching international statistical outcomes regarding midwifery vs. obstetrical care, midwives have far exceeded the lower infant mortality rates, fewer medical interventions and higher results in more empowering births. A concern regarding water labor or birth is infection. When in the water, bacteria is diluted. Unless someone enters the water with an infection of some sort offering foreign bacteria, there wouldn’t be problems with the mothers infecting herself or the baby. A study in 1996 of 1385 women with prelabor rupture of the membranes after 34 weeks gestation concluded a tub bath did not increase the risk of maternal or neonatal infection after premature rupture of the membranes and prolonged latency. (1)
A concern regarding water labor or birth is infection. When in the water, bacteria is diluted. Unless someone enters the water with an infection of some sort offering foreign bacteria, there wouldn’t be problems with the mothers infecting herself or the baby. A study in 1996 of 1385 women with prelabor rupture of the membranes after 34 weeks gestation concluded a tub bath did not increase the risk of maternal or neonatal infection after premature rupture of the membranes and prolonged latency. (1)
 in a nursing school and continued until she got sick and decided to become an independent midwife.
in a nursing school and continued until she got sick and decided to become an independent midwife. The labor and birth area, downstairs, contains an aqua blue oval tub, covered with a sterile plastic cover, weighted down by sterling sliver dolphin, moon and starburst clips, keeping the tub clean and available to use at any time. The tub is next to a cluttered desk, a bed that rotates up and down, colorful bean bags to sit or lean on, a short low birth chair, a geriatric stool to lean over with a hidden foam pad which Yamada quickly retrieves from under the bed. With a press of a button a heat a toilet is seated. With a press of a few more buttons a genital area is washed and dried automatically. Ah, the wonders of another country. Yamada believes in low light levels and keeps the overhead lights off and the decorative side wall lights on. Midwives utilize an underwater doppler stethoscope to check the babies heart tones. The house includes steep staircases, a modest kitchen, an additional room with a jacuzzi tub, areas for weighing, bathing and checking the jaundice levels of the babies.
The labor and birth area, downstairs, contains an aqua blue oval tub, covered with a sterile plastic cover, weighted down by sterling sliver dolphin, moon and starburst clips, keeping the tub clean and available to use at any time. The tub is next to a cluttered desk, a bed that rotates up and down, colorful bean bags to sit or lean on, a short low birth chair, a geriatric stool to lean over with a hidden foam pad which Yamada quickly retrieves from under the bed. With a press of a button a heat a toilet is seated. With a press of a few more buttons a genital area is washed and dried automatically. Ah, the wonders of another country. Yamada believes in low light levels and keeps the overhead lights off and the decorative side wall lights on. Midwives utilize an underwater doppler stethoscope to check the babies heart tones. The house includes steep staircases, a modest kitchen, an additional room with a jacuzzi tub, areas for weighing, bathing and checking the jaundice levels of the babies. washing the baby in the bath before they leave the House. Yamada teaches only the father how to bathe the baby, not the mother. This is a way to establish a special commitment from the father in his assistance and caregiving for the child. The bath is not given the first day of the birth, only the second day after. Every day Yamada checks the babies jaundice with a small, handheld portable machine.
washing the baby in the bath before they leave the House. Yamada teaches only the father how to bathe the baby, not the mother. This is a way to establish a special commitment from the father in his assistance and caregiving for the child. The bath is not given the first day of the birth, only the second day after. Every day Yamada checks the babies jaundice with a small, handheld portable machine. Yamada’s assistant and midwife in training, Ms. Megumi Tanaki was seven months pregnant when I did the interview. Tanaki’s background as a nurse for many years in a private hospital and University Medical Hospital left her feeling limited as a nurse. Tanaki shares, “When I worked as a shift nurse and the Hospital became bigger and bigger, I wasn’t able to manage what I wanted to do as a nurse because it is institutionalized and I had to work as a group organization.”
Yamada’s assistant and midwife in training, Ms. Megumi Tanaki was seven months pregnant when I did the interview. Tanaki’s background as a nurse for many years in a private hospital and University Medical Hospital left her feeling limited as a nurse. Tanaki shares, “When I worked as a shift nurse and the Hospital became bigger and bigger, I wasn’t able to manage what I wanted to do as a nurse because it is institutionalized and I had to work as a group organization.” babies, my physical balance is quite good. I believe my hormones become more balanced when I assist the births with the mothers and babies. I work in good circumstances so this is my happiness,” concludes Tanaki.
babies, my physical balance is quite good. I believe my hormones become more balanced when I assist the births with the mothers and babies. I work in good circumstances so this is my happiness,” concludes Tanaki.



 If you are fortunate enough to be invited into the OR in a hospital,
If you are fortunate enough to be invited into the OR in a hospital,
 BB © 2013
BB © 2013 During the early 1980s, Estelle Myers, at the Rainbow Dolphin Centre in New Zealand, led the first two waterbirth conferences.
During the early 1980s, Estelle Myers, at the Rainbow Dolphin Centre in New Zealand, led the first two waterbirth conferences.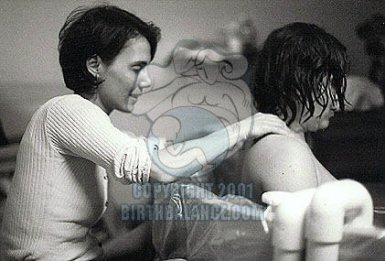 Doula Linda Cohen in Long Island, New York devised a rather simple recipe for situations in the hospital where the mother is not allowed anything but ice chips and water. She calls this “The Drizzle.” In a cup add: a bit of infused (very strong) hot red raspberry leaf tea and a teaspoon of honey; mix thoroughly and add ice chips. Feed to mother with a spoon while in the tub, on the birth throne (toilet), on a bed, kneeling over a physioball, walking down the hall or up and down stairwells. Once I was fortunate enough to be invited to a home birth with a small group of Russians from Moscow. I saw a small bowl of fresh cranberries on the side of the tub. Periodically the mother would suck on one, put it back in the bowl and go through the contraction. Sucking the cranberries, the mother claimed, helped stimulate her thirst. As an assistant, I periodically ask the mother if the water feels too cool or too warm. Placing a small thermometer in the tub helps monitor the temperature. If the water is too hot and the mother desires it to be even warmer, I suggest she get out of the water and walk. If the water became too cold I would add hot water away from the mother if she remains in the tub or get her out of the tub and add the water. Another trick the Russians taught me is, if the mother is feeling too warm in the tub yet doesn’t want to get out, she can hold onto pieces of ice to cool down, or sit along the edge of the tub with her feet still in the water. Barbara Harper explains: “The greatest benefit to immersion will be experienced in the first hour to two hours. Twenty minutes in the bath is not enough for the physiologic responses to work effectively. That is why some women, both primips and multips, get into the water at 7 cm or 8 cm dilation and begin to experience pushing urges within the first hour of immersion.”
Doula Linda Cohen in Long Island, New York devised a rather simple recipe for situations in the hospital where the mother is not allowed anything but ice chips and water. She calls this “The Drizzle.” In a cup add: a bit of infused (very strong) hot red raspberry leaf tea and a teaspoon of honey; mix thoroughly and add ice chips. Feed to mother with a spoon while in the tub, on the birth throne (toilet), on a bed, kneeling over a physioball, walking down the hall or up and down stairwells. Once I was fortunate enough to be invited to a home birth with a small group of Russians from Moscow. I saw a small bowl of fresh cranberries on the side of the tub. Periodically the mother would suck on one, put it back in the bowl and go through the contraction. Sucking the cranberries, the mother claimed, helped stimulate her thirst. As an assistant, I periodically ask the mother if the water feels too cool or too warm. Placing a small thermometer in the tub helps monitor the temperature. If the water is too hot and the mother desires it to be even warmer, I suggest she get out of the water and walk. If the water became too cold I would add hot water away from the mother if she remains in the tub or get her out of the tub and add the water. Another trick the Russians taught me is, if the mother is feeling too warm in the tub yet doesn’t want to get out, she can hold onto pieces of ice to cool down, or sit along the edge of the tub with her feet still in the water. Barbara Harper explains: “The greatest benefit to immersion will be experienced in the first hour to two hours. Twenty minutes in the bath is not enough for the physiologic responses to work effectively. That is why some women, both primips and multips, get into the water at 7 cm or 8 cm dilation and begin to experience pushing urges within the first hour of immersion.”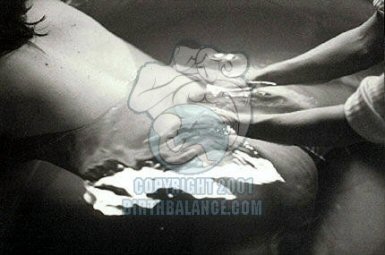 In Bristol, two women who had adverse perinatal outcomes had labored for more than seven hours in the birthing pool. There was one stillborn child with evidence of asphyxia and one baby with severe hypoxic-ischaemic encephalopathy. These women had labored, not birthed in the water. In neither case was any specific cause evident.
In Bristol, two women who had adverse perinatal outcomes had labored for more than seven hours in the birthing pool. There was one stillborn child with evidence of asphyxia and one baby with severe hypoxic-ischaemic encephalopathy. These women had labored, not birthed in the water. In neither case was any specific cause evident.  In regard to the physiology of birth, each woman responds differently to pain, yet when mothers get into the water, there is a universal, “AhhhhŠoh my god, why did I wait so long!” After the tenth person responded with the exact words, I wondered if I was experiencing the “hundredth monkey” concept. Barbara Harper, director of Global Maternal Child/Health Association, reports on her survey of close to 2,000 women, when asked the question, “What feelings do you recall?”‹almost 100 percent of women stated in one form or another they were relaxed, calm, at peace in the water.
In regard to the physiology of birth, each woman responds differently to pain, yet when mothers get into the water, there is a universal, “AhhhhŠoh my god, why did I wait so long!” After the tenth person responded with the exact words, I wondered if I was experiencing the “hundredth monkey” concept. Barbara Harper, director of Global Maternal Child/Health Association, reports on her survey of close to 2,000 women, when asked the question, “What feelings do you recall?”‹almost 100 percent of women stated in one form or another they were relaxed, calm, at peace in the water.