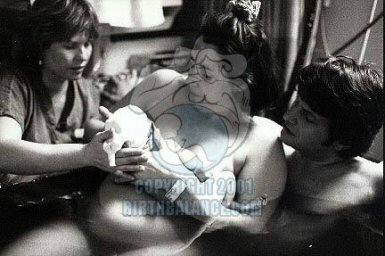
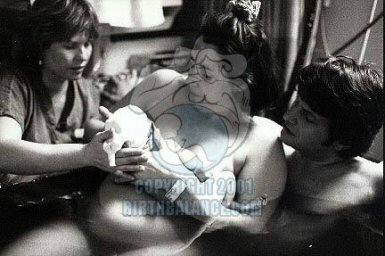
In an ancient tradition of “woman supporting woman,” my friend asked me to do something I’d never done before attend the birth of a child. “Just be there and support me, massage me, talk to me,” she said, then added matter-of-factly: “Oh, by the way, we’re going to have the baby underwater.” It was a cold, blustery evening in November 1987 when baby Maxx appeared, landmarking the first home underwater birth in New York City accompanied by a midwife. Thus was conceived my passion for birth. Without much information available to us at that time, we were all virgins finding our way as comfortably as possible to fulfill the mother’s wishes. We had three resources: books by Erik Sidenbladh1, Timothy Wyllie2 and Dr. Michel Odent.3 In 1987 very few if any hospitals in the United States had birthing tubs. In 1996 a handful of U.S. hospitals offered birthing tubs; today hundreds do. Waterbirth, which started in Russia during the 1950s and 1960s, moved to France and England in the 1970s and to America in the mid-1980s, was once considered a fad. Today it has become the “aquadural,” replacing for many women the epidural. Innovative and controversial, the aquadural involves laboring and/or birthing under water. After my initiation in 1987, I became one of the first of a handful of doulas in New York City. The doula, a specialist in labor, has become another significant element in late twentieth and early twenty-first century birth, one that decreases the need for drugs, interventions and surgical procedures up to 50 percent. 4 A “douladural” is a non-medical person who has certification training or life experience in the birth field. She acts as a liaison between medical caregivers and parents by offering physical, mental, emotional and spiritual support. She does not perform medical procedures or make medical decisions, yet she does advise the parents on these matters.
Safety Reports and Stipulations
 During the early 1980s, Estelle Myers, at the Rainbow Dolphin Centre in New Zealand, led the first two waterbirth conferences.5 International waterbirth conferences were held in London, England in 1995 and Greensboro, North Carolina in 1996. Thousands of births reported at these conferences confirmed no increase of infection to baby or mother or fetal or maternal deaths due to the water. 6 The next international waterbirth conference will be held in Portland, Oregon in September 2000 and is co-sponsored by Midwifery Today.
During the early 1980s, Estelle Myers, at the Rainbow Dolphin Centre in New Zealand, led the first two waterbirth conferences.5 International waterbirth conferences were held in London, England in 1995 and Greensboro, North Carolina in 1996. Thousands of births reported at these conferences confirmed no increase of infection to baby or mother or fetal or maternal deaths due to the water. 6 The next international waterbirth conference will be held in Portland, Oregon in September 2000 and is co-sponsored by Midwifery Today.
In the late 1980s to mid-1990s, a series of articles in the medical journals noted the death of a baby in Sweden, one death and one brain-damaged baby in Britain and one death in France due to water labor or birth. After further investigations, it was shown that the water was not the cause of these babies’ deaths and brain damage; rather, other mitigating circumstances were evident. 7 As a result of these incidents the following stipulations occurred and were administered: 1) decrease the temperature of the water to body temperature‹ 97 to 99 degrees Fahrenheit or 34 to 38 Celsius; 2) encourage the mother to get in the water no earlier than five centimeters dilated; 3) shorten the labor time a mother is in the tub; 4) shorten the amount of time the baby is submerged. The Royal Society of Medicine delivered an abstract on a comparison of 602 maternal and neonatal outcomes in waterbirths and conventional vaginal deliveries from 1989 to 1994 (301 women electing for waterbirths compared with the same number of age- and parity-matched low-risk women having conventional vaginal deliveries). The Society¹s conclusion: waterbirths in low-risk women delivered by experienced professionals are as safe as normal deliveries. Laboring and delivering in water is associated with a reduction in length of labor and perineal trauma for primigravidae and a reduction in analgesia requirements for all women. If a mother is in a prodromal labor pattern early on, having intense back-to-back contractions with a two to three centimeter dilation, she can become extremely tired. I suggest she sit in the tub for therapeutic rest and encouragement. If the temperature exceeds 99º F or 38º C, it can lead to hyperthermia and dehydration in the mother and baby. It is also imperative that the mother as well as the assistants in the room drink fluids with glucose. If the mother is not well hydrated, it leads to low blood volume and could possibly result in orthostatic hypertension, passing out when standing up to get out of the pool.9 Janet Balaskas states in her book, Water Birth: Maintaining the correct water temperature is very important. If the water temperature is too low the mother’s body temperature particularly if she spends a long time in the pool, will drop. The sweating mechanism for heat loss does not work in water, so if the water is too warm the mother’s body temperature will rise and her energy may be sapped. 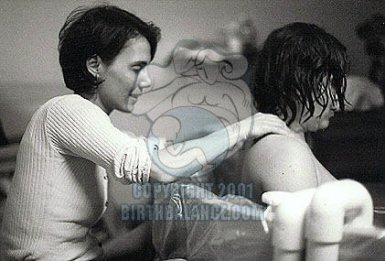 Doula Linda Cohen in Long Island, New York devised a rather simple recipe for situations in the hospital where the mother is not allowed anything but ice chips and water. She calls this “The Drizzle.” In a cup add: a bit of infused (very strong) hot red raspberry leaf tea and a teaspoon of honey; mix thoroughly and add ice chips. Feed to mother with a spoon while in the tub, on the birth throne (toilet), on a bed, kneeling over a physioball, walking down the hall or up and down stairwells. Once I was fortunate enough to be invited to a home birth with a small group of Russians from Moscow. I saw a small bowl of fresh cranberries on the side of the tub. Periodically the mother would suck on one, put it back in the bowl and go through the contraction. Sucking the cranberries, the mother claimed, helped stimulate her thirst. As an assistant, I periodically ask the mother if the water feels too cool or too warm. Placing a small thermometer in the tub helps monitor the temperature. If the water is too hot and the mother desires it to be even warmer, I suggest she get out of the water and walk. If the water became too cold I would add hot water away from the mother if she remains in the tub or get her out of the tub and add the water. Another trick the Russians taught me is, if the mother is feeling too warm in the tub yet doesn’t want to get out, she can hold onto pieces of ice to cool down, or sit along the edge of the tub with her feet still in the water. Barbara Harper explains: “The greatest benefit to immersion will be experienced in the first hour to two hours. Twenty minutes in the bath is not enough for the physiologic responses to work effectively. That is why some women, both primips and multips, get into the water at 7 cm or 8 cm dilation and begin to experience pushing urges within the first hour of immersion.”11 Keeping a woman in the water for hours is unsafe and unnecessary. I just received a call from a mother who labored in a rented tub at home but didn’t birth there. I asked her why not. She responded: “The water was filthy after being in it for six hours and by the time we had drained it and started to fill it again, the baby was born.”
Doula Linda Cohen in Long Island, New York devised a rather simple recipe for situations in the hospital where the mother is not allowed anything but ice chips and water. She calls this “The Drizzle.” In a cup add: a bit of infused (very strong) hot red raspberry leaf tea and a teaspoon of honey; mix thoroughly and add ice chips. Feed to mother with a spoon while in the tub, on the birth throne (toilet), on a bed, kneeling over a physioball, walking down the hall or up and down stairwells. Once I was fortunate enough to be invited to a home birth with a small group of Russians from Moscow. I saw a small bowl of fresh cranberries on the side of the tub. Periodically the mother would suck on one, put it back in the bowl and go through the contraction. Sucking the cranberries, the mother claimed, helped stimulate her thirst. As an assistant, I periodically ask the mother if the water feels too cool or too warm. Placing a small thermometer in the tub helps monitor the temperature. If the water is too hot and the mother desires it to be even warmer, I suggest she get out of the water and walk. If the water became too cold I would add hot water away from the mother if she remains in the tub or get her out of the tub and add the water. Another trick the Russians taught me is, if the mother is feeling too warm in the tub yet doesn’t want to get out, she can hold onto pieces of ice to cool down, or sit along the edge of the tub with her feet still in the water. Barbara Harper explains: “The greatest benefit to immersion will be experienced in the first hour to two hours. Twenty minutes in the bath is not enough for the physiologic responses to work effectively. That is why some women, both primips and multips, get into the water at 7 cm or 8 cm dilation and begin to experience pushing urges within the first hour of immersion.”11 Keeping a woman in the water for hours is unsafe and unnecessary. I just received a call from a mother who labored in a rented tub at home but didn’t birth there. I asked her why not. She responded: “The water was filthy after being in it for six hours and by the time we had drained it and started to fill it again, the baby was born.” 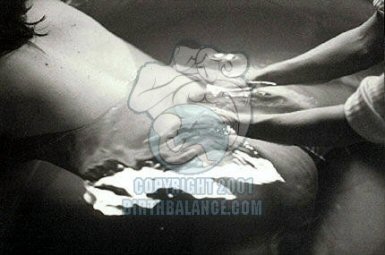 In Bristol, two women who had adverse perinatal outcomes had labored for more than seven hours in the birthing pool. There was one stillborn child with evidence of asphyxia and one baby with severe hypoxic-ischaemic encephalopathy. These women had labored, not birthed in the water. In neither case was any specific cause evident. 12 When helping the woman out of the water, one must be aware of the “fetus ejection reflex,” a term coined by Dr. Michel Odent. 13 This means there is a possibility of the baby slipping through the birth canal unexpectedly because of the change of atmospheric pressure and movement. I focus on the laboring mother¹s pelvic area and keep in touch with the physical sensations she is feeling when assisting her out of the tub. I also make sure if in a birth center or hospital, to wrap the mother in the kind of warm large white thin blanket supplied by the hospital or birth center. I use the small towels to wipe the legs and feet of the shivering woman stepping out of the water. I also make sure the room temperature is as warm as possible so the mother does not chill from water to air. In some facilities, especially hospitals, we have no direct control of the temperature. Most facilities are quite cold. In one hospital we fooled the thermostat by taking a rubber glove, filling it with ice chips, slipping a knot at the opening of the wrist and placing the dangling fingers of ice on the thermostat box. Worked like a charm. It is also important the mother does not slip when exiting the tub. I think it’s a good idea to put a large tarp underneath the portable tub. Towels placed on the floor beside the entrance to the tub help create an absorbent, non-slip surface. If there is full access around the tub, I place towels around the whole area. When a baby completely emerges from the womb it is logical to get the child directly into the mother¹s arms, or better, to assist the mother as she brings the baby to her belly or chest. Oxygen flows to the baby through the umbilical cord attached to the placenta. When the placenta detaches completely or partially from the mother, the baby¹s supply of oxygen is compromised. Thus emergence within a short time is of essence. There was a case during the early 1980s in the United States where a couple, unattended by medical caregivers, left their child under the water after the placenta was birthed. The baby died due to lack of oxygen. 14 When pulling the baby out of the water and onto the mother’s belly or chest, it is important to become aware of the length of the umbilical cord. It’s easy to snap a short cord if one pulls the baby up abruptly.
In Bristol, two women who had adverse perinatal outcomes had labored for more than seven hours in the birthing pool. There was one stillborn child with evidence of asphyxia and one baby with severe hypoxic-ischaemic encephalopathy. These women had labored, not birthed in the water. In neither case was any specific cause evident. 12 When helping the woman out of the water, one must be aware of the “fetus ejection reflex,” a term coined by Dr. Michel Odent. 13 This means there is a possibility of the baby slipping through the birth canal unexpectedly because of the change of atmospheric pressure and movement. I focus on the laboring mother¹s pelvic area and keep in touch with the physical sensations she is feeling when assisting her out of the tub. I also make sure if in a birth center or hospital, to wrap the mother in the kind of warm large white thin blanket supplied by the hospital or birth center. I use the small towels to wipe the legs and feet of the shivering woman stepping out of the water. I also make sure the room temperature is as warm as possible so the mother does not chill from water to air. In some facilities, especially hospitals, we have no direct control of the temperature. Most facilities are quite cold. In one hospital we fooled the thermostat by taking a rubber glove, filling it with ice chips, slipping a knot at the opening of the wrist and placing the dangling fingers of ice on the thermostat box. Worked like a charm. It is also important the mother does not slip when exiting the tub. I think it’s a good idea to put a large tarp underneath the portable tub. Towels placed on the floor beside the entrance to the tub help create an absorbent, non-slip surface. If there is full access around the tub, I place towels around the whole area. When a baby completely emerges from the womb it is logical to get the child directly into the mother¹s arms, or better, to assist the mother as she brings the baby to her belly or chest. Oxygen flows to the baby through the umbilical cord attached to the placenta. When the placenta detaches completely or partially from the mother, the baby¹s supply of oxygen is compromised. Thus emergence within a short time is of essence. There was a case during the early 1980s in the United States where a couple, unattended by medical caregivers, left their child under the water after the placenta was birthed. The baby died due to lack of oxygen. 14 When pulling the baby out of the water and onto the mother’s belly or chest, it is important to become aware of the length of the umbilical cord. It’s easy to snap a short cord if one pulls the baby up abruptly.  In regard to the physiology of birth, each woman responds differently to pain, yet when mothers get into the water, there is a universal, “AhhhhŠoh my god, why did I wait so long!” After the tenth person responded with the exact words, I wondered if I was experiencing the “hundredth monkey” concept. Barbara Harper, director of Global Maternal Child/Health Association, reports on her survey of close to 2,000 women, when asked the question, “What feelings do you recall?”‹almost 100 percent of women stated in one form or another they were relaxed, calm, at peace in the water. 15 I can say that for every birth I’ve attended where there was a tub of water and a challenging labor or birth, that without the water, the woman would have received an epidural. During one of my interviews for my local cable program, Birth Balance Presents: Waterbirth, I was interviewing a mother who labored in water and birthed her baby in air due to meconium and late due date. When I commented to her, “From my observations of you during the labor, if you had not had the tub available, I believe there was an 80 percent chance you would have gotten an epidural.” “Eighty!” she exclaimed, “200 percent I would have gotten the epidural! The water saved me.” When sticking my hands in the water to massage or support I do not wear gloves. I wash thoroughly with antiseptic soap and make sure I do not have any staph infections on my body. In one case an infection was passed to the baby during a water labor because the father had a staph infection on his foot and was in the water when the baby was born. When I am pressing points on the mother’s back during a contraction or massaging her shoulders, legs or belly in between contractions, the warm water soothes my tired hands and arms. I am also given more breaks from actual hands on at a water labor because the women spend time rocking back and forth on their hands and knees moaning and breathing. This gives me time to talk gently to a birthing mother or massage the father. During my prenatal visits with parents to discuss their birth plans and choices for childbirth, I encourage them to stay open and unattached to birthing in the water. Waterbirth should not be the goal. Often times when a woman becomes fixated on any particular outcome of birth, there potentially are more difficulties because of inflexibility. Dr. Michel Odent speaks often of women getting out of the tubs right when they are to push their babies out, so that they then present right alongside the tub. Or when the water is running into the tub, the woman may grab alongside the tub and begin to scream as her contractions become stronger. In some cases, women actually birth their babies just by the sound of the water running. Listening to one’s body, trusting the process and going with the flow are vital. A question I am commonly asked is: “Is it a good idea to hire a doula who has little or no experience with water labor or birth?” In this day and age, there is so much information about this alternative method of labor and birth. If the doula is more inexperienced it would be worth her time to research through the Internet, read books, watch and listen to video and audiotapes. Anyone can read up, ask questions, talk to parents who’ve had a water labor or birth, and attend lectures or private consultations with a waterbirth consultant. It is more important that parents have a strong connection with the doula they have interviewed. Educating and participating is a moment to moment experience.
In regard to the physiology of birth, each woman responds differently to pain, yet when mothers get into the water, there is a universal, “AhhhhŠoh my god, why did I wait so long!” After the tenth person responded with the exact words, I wondered if I was experiencing the “hundredth monkey” concept. Barbara Harper, director of Global Maternal Child/Health Association, reports on her survey of close to 2,000 women, when asked the question, “What feelings do you recall?”‹almost 100 percent of women stated in one form or another they were relaxed, calm, at peace in the water. 15 I can say that for every birth I’ve attended where there was a tub of water and a challenging labor or birth, that without the water, the woman would have received an epidural. During one of my interviews for my local cable program, Birth Balance Presents: Waterbirth, I was interviewing a mother who labored in water and birthed her baby in air due to meconium and late due date. When I commented to her, “From my observations of you during the labor, if you had not had the tub available, I believe there was an 80 percent chance you would have gotten an epidural.” “Eighty!” she exclaimed, “200 percent I would have gotten the epidural! The water saved me.” When sticking my hands in the water to massage or support I do not wear gloves. I wash thoroughly with antiseptic soap and make sure I do not have any staph infections on my body. In one case an infection was passed to the baby during a water labor because the father had a staph infection on his foot and was in the water when the baby was born. When I am pressing points on the mother’s back during a contraction or massaging her shoulders, legs or belly in between contractions, the warm water soothes my tired hands and arms. I am also given more breaks from actual hands on at a water labor because the women spend time rocking back and forth on their hands and knees moaning and breathing. This gives me time to talk gently to a birthing mother or massage the father. During my prenatal visits with parents to discuss their birth plans and choices for childbirth, I encourage them to stay open and unattached to birthing in the water. Waterbirth should not be the goal. Often times when a woman becomes fixated on any particular outcome of birth, there potentially are more difficulties because of inflexibility. Dr. Michel Odent speaks often of women getting out of the tubs right when they are to push their babies out, so that they then present right alongside the tub. Or when the water is running into the tub, the woman may grab alongside the tub and begin to scream as her contractions become stronger. In some cases, women actually birth their babies just by the sound of the water running. Listening to one’s body, trusting the process and going with the flow are vital. A question I am commonly asked is: “Is it a good idea to hire a doula who has little or no experience with water labor or birth?” In this day and age, there is so much information about this alternative method of labor and birth. If the doula is more inexperienced it would be worth her time to research through the Internet, read books, watch and listen to video and audiotapes. Anyone can read up, ask questions, talk to parents who’ve had a water labor or birth, and attend lectures or private consultations with a waterbirth consultant. It is more important that parents have a strong connection with the doula they have interviewed. Educating and participating is a moment to moment experience.
Click to View Judith Halek’s toolbaghttp://www.birthbalance.com/articles/toolbag.asp
Judith Elaine Halek is the founder and director of Birth Balance, an East Coast resource center for underwater birth that she started in 1987. One of the original labor support doulas in New York City, she has pioneered alternative choices in childbirth throughout the tri-state area. A birth consultant and counselor, massage and fitness therapist, writer, educator, speaker, photographer, videographer and producer of Birth Balance Presents: Water Birth, a Manhattan Educational Cable Station, Judith is airing her third thirteen-part weekly series on underwater birth and midwifery related issues. If you would like to contact Judith directly by email she’s at: Judith@BirthBalance.com.
Footnotes
1. Sidenbladh, E. (1982). Water Babies, A Book about Igor Tjarkovsky and His Method for Delivering and Training Children in Water. New York City: St. Martin’s Press. 2. Wyllie, T. (1984). Dolphins, Extraterrestrials, Angels, Adventures among Spiritual Intelligences. Boston Enterprises (distributed by Knoll Publishing Company, IN). 3. Odent, M. (1983). Birth under water. Lancet 2:1776-1477. 4. Klaus, M.H. & Kennell, J.H. & Klaus, P.H. (1993). Mothering the Mother, How a Doula Can Help You Have a Shorter, Easier, and Healthier Birth. New York City: Addison-Wesley. 5. Myers, E. (1976, 1999). Cross Your Bridges When You Come to Them. New Zealand: Rainbow Dolphin Centre. 6. Beech, B.L. (1996). Water Birth Unplugged, Proceedings of the First International Water Birth Conference. England: Books For Midwives Press. 7. Ingrey, J. (1993). Water birth press release. Midwifery Matters, Issue 59, Winter. 8. Royal Society of Medicine. A Comparison of Maternal and Neonatal Outcome in Water Births and Conventional Vaginal Deliveries. C171-29C-2986, p.10. 9. Harper, B. (1999). Water birth report. OBC News. 10. Balaskas, J. & Gordon Y. (1990). Water Birth, The Concise Guide to Using Water during Pregnancy Birth and Infancy. Great Britain: Unwin Hyman LTD. 11. Harper, B. (1999). Ibid. 12. Gilbert, R.E. & Tookey, P.A. (1999, Aug. 21). Perinatal mortality and morbidity among babies delivered in water: surveillance study and postal survey. BMJ 319-483. 13. Odent, M. (1987). The fetus ejection reflex. Birth 12(2). 14. Ingrey, J. (1993). Ibid. 15. Harper, B. (1999). Ibid. 16. Napierala, S. (1994). Waterbirth, A Midwives Perspective. Connecticut: Bergin & Garvey (a branch of Greenwood Pub. Inc.). 17. Lichy, R. & Herzberg, E. (1993). The Waterbirth Handbook, The Gentle Art of Waterbirthing. United Kingdom: Gateway Books. 18. Balaskas, J. & Gordon Y. (1990). Water Birth, The Concise Guide to Using Water during Pregnancy Birth and Infancy. Great Britain: Unwin Hyman LTD.
Additional Resources
Gilbert, R.E. & Tookey, P.A. (1999, Aug. 21). Perinatal mortality and morbidity among babies delivered in water: Surveillance study and postal survey. British Medical Journal. 319:483-487.www.bmj.com/cgi/content/abstract/319/7208/483 under Obstetrics and Gynecology: Pregnancy. The conclusions from this paper: “Perinatal mortality is not substantially higher among babies delivered in water than among those born to low risk women who delivered conventionally. The data are compatible with a small increase or decrease in perinatal mortality for babies in water.” I have also found the waterbirth egroups, a group of like-minded people who share and question and learn more about waterbirth, to be informative and educational. To register: www.egroups.com/subscribe/waterbirth An online electronic Waterbirth Newsletter is debuting in April 2000. To subscribe: www.egroups.com/subscribe/WaterbirthNews

 scooper for scooping out fecal and birth matter released in the water during labor or birth, they purchase one from a local pet store, sterilize it and wrap it in a plastic Ziploc. Urinating in the water is fine. Urine is sterile and clearing the bladder will make room for the babies’ head to dip down. I suggest, however, that all labor attendants in the water use the bathroom facilities.
scooper for scooping out fecal and birth matter released in the water during labor or birth, they purchase one from a local pet store, sterilize it and wrap it in a plastic Ziploc. Urinating in the water is fine. Urine is sterile and clearing the bladder will make room for the babies’ head to dip down. I suggest, however, that all labor attendants in the water use the bathroom facilities.
 BB © 2013
BB © 2013 During the early 1980s, Estelle Myers, at the Rainbow Dolphin Centre in New Zealand, led the first two waterbirth conferences.
During the early 1980s, Estelle Myers, at the Rainbow Dolphin Centre in New Zealand, led the first two waterbirth conferences.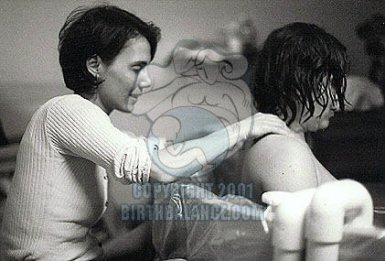 Doula Linda Cohen in Long Island, New York devised a rather simple recipe for situations in the hospital where the mother is not allowed anything but ice chips and water. She calls this “The Drizzle.” In a cup add: a bit of infused (very strong) hot red raspberry leaf tea and a teaspoon of honey; mix thoroughly and add ice chips. Feed to mother with a spoon while in the tub, on the birth throne (toilet), on a bed, kneeling over a physioball, walking down the hall or up and down stairwells. Once I was fortunate enough to be invited to a home birth with a small group of Russians from Moscow. I saw a small bowl of fresh cranberries on the side of the tub. Periodically the mother would suck on one, put it back in the bowl and go through the contraction. Sucking the cranberries, the mother claimed, helped stimulate her thirst. As an assistant, I periodically ask the mother if the water feels too cool or too warm. Placing a small thermometer in the tub helps monitor the temperature. If the water is too hot and the mother desires it to be even warmer, I suggest she get out of the water and walk. If the water became too cold I would add hot water away from the mother if she remains in the tub or get her out of the tub and add the water. Another trick the Russians taught me is, if the mother is feeling too warm in the tub yet doesn’t want to get out, she can hold onto pieces of ice to cool down, or sit along the edge of the tub with her feet still in the water. Barbara Harper explains: “The greatest benefit to immersion will be experienced in the first hour to two hours. Twenty minutes in the bath is not enough for the physiologic responses to work effectively. That is why some women, both primips and multips, get into the water at 7 cm or 8 cm dilation and begin to experience pushing urges within the first hour of immersion.”
Doula Linda Cohen in Long Island, New York devised a rather simple recipe for situations in the hospital where the mother is not allowed anything but ice chips and water. She calls this “The Drizzle.” In a cup add: a bit of infused (very strong) hot red raspberry leaf tea and a teaspoon of honey; mix thoroughly and add ice chips. Feed to mother with a spoon while in the tub, on the birth throne (toilet), on a bed, kneeling over a physioball, walking down the hall or up and down stairwells. Once I was fortunate enough to be invited to a home birth with a small group of Russians from Moscow. I saw a small bowl of fresh cranberries on the side of the tub. Periodically the mother would suck on one, put it back in the bowl and go through the contraction. Sucking the cranberries, the mother claimed, helped stimulate her thirst. As an assistant, I periodically ask the mother if the water feels too cool or too warm. Placing a small thermometer in the tub helps monitor the temperature. If the water is too hot and the mother desires it to be even warmer, I suggest she get out of the water and walk. If the water became too cold I would add hot water away from the mother if she remains in the tub or get her out of the tub and add the water. Another trick the Russians taught me is, if the mother is feeling too warm in the tub yet doesn’t want to get out, she can hold onto pieces of ice to cool down, or sit along the edge of the tub with her feet still in the water. Barbara Harper explains: “The greatest benefit to immersion will be experienced in the first hour to two hours. Twenty minutes in the bath is not enough for the physiologic responses to work effectively. That is why some women, both primips and multips, get into the water at 7 cm or 8 cm dilation and begin to experience pushing urges within the first hour of immersion.”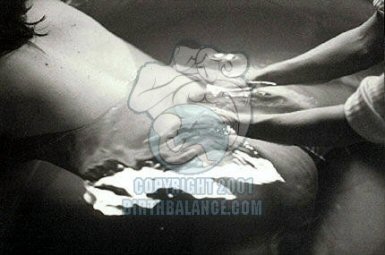 In Bristol, two women who had adverse perinatal outcomes had labored for more than seven hours in the birthing pool. There was one stillborn child with evidence of asphyxia and one baby with severe hypoxic-ischaemic encephalopathy. These women had labored, not birthed in the water. In neither case was any specific cause evident.
In Bristol, two women who had adverse perinatal outcomes had labored for more than seven hours in the birthing pool. There was one stillborn child with evidence of asphyxia and one baby with severe hypoxic-ischaemic encephalopathy. These women had labored, not birthed in the water. In neither case was any specific cause evident.  In regard to the physiology of birth, each woman responds differently to pain, yet when mothers get into the water, there is a universal, “AhhhhŠoh my god, why did I wait so long!” After the tenth person responded with the exact words, I wondered if I was experiencing the “hundredth monkey” concept. Barbara Harper, director of Global Maternal Child/Health Association, reports on her survey of close to 2,000 women, when asked the question, “What feelings do you recall?”‹almost 100 percent of women stated in one form or another they were relaxed, calm, at peace in the water.
In regard to the physiology of birth, each woman responds differently to pain, yet when mothers get into the water, there is a universal, “AhhhhŠoh my god, why did I wait so long!” After the tenth person responded with the exact words, I wondered if I was experiencing the “hundredth monkey” concept. Barbara Harper, director of Global Maternal Child/Health Association, reports on her survey of close to 2,000 women, when asked the question, “What feelings do you recall?”‹almost 100 percent of women stated in one form or another they were relaxed, calm, at peace in the water.