
By Judith Elaine Halek
Photos and Article Copyright @ 2000 Judith Elaine Halek
I was sitting at a dinner table with a group of women in their late thirties and forties. I, myself, am in my early forty’s, not married, been working in the birth modalities for the past twelve years and at present, am not seeing anyone in particular. I commented, “I don’t think it’s in the cards for me to have a baby this lifetime.””Really!” exclaimed a couple of the women. “How old are you?” inquired one woman. “Close to my mid forties.” I responded. “Oh, that won’t be a problem,” she said matter of factly, “You can always do invitro, or donor insemination.” I looked at her and then to other women around the table as all eyes were set on my response. I was surprised and disappointed that conception has become a casual ‘technocratic procedure’ in the minds of the public. I began to explain IVF and donor insemination requires massive douses of antibiotics, a large bank account, arranging one’s work schedule around clinic visits, undergoing countless invasive, often painful, always emotionally charged procedures, all for the chance that I might be the one of ten to be blessed with the news of a cyborg conception. Please understand, I am not judging anyone who chooses this path of conception. It is not my preference of choice and thank goodness, we still have a choice.
Or do we? When I reflect back on my experiences the past twelve years as a labor support specialist, childbirth educator, birth counselor, massage therapist, yoga instructor I’ve found far too many women who did not exercise their options of choice and gave their power away to the medical caregivers, especially in hospitals. After attending over 100 births in hospitals, birth centers and homes, I have had the opportunity to experience a variety of possibilities. It is my vision, that all labor and delivery nurses and obstetricians witness 30 home births or birth center births as part of their medical training.
|
I remember at one hospital, a nurse commented, “Having a baby at home is one of the most dangerous experiences a mother could put her baby and herself through.” I asked if she had ever attended a home birth, or studied the statistics of home birth practices. She admitted she had not attended a one or knew anything about recent studies on home birthwith midwife practices. I asked her, as I’ve asked many people who make blanket statements without any information to back up their claims, “How can you make such a definitive comment when you’ve not any experience with what you are judging?” |
It’s rather ironic that we in our intellectual aspects, read, watch videos, attend classes, surf the internet, express our gathering feminine nature, becoming an ‘informed consumer’, yet when it all comes down to the real deal, one of my favorite mentors, Dr. Michel Odent states, “Forget the books, tapes, videos. Go to a quiet, dark place, private and safe, trust the process, surrender to your bodies and have your babies.”
I believe women have forgotten how to birth, trust, listen, go deep inside and communicate with their bodies and their babies. I also believe women can remember.
What are the choices, options, for non-technocratic pregnancies, labors and births? I have been an advocate of midwifery for the past 12 years. After researching international statistical outcomes regarding midwifery vs. obstetrical care, midwives have far exceeded the lower infant mortality rates, fewer medical interventions and higher results in more empowering births.
been an advocate of midwifery for the past 12 years. After researching international statistical outcomes regarding midwifery vs. obstetrical care, midwives have far exceeded the lower infant mortality rates, fewer medical interventions and higher results in more empowering births.
Having a baby with an obstetrition in a hospital? Create a birth plan, a “guide line,” toward the ideal birth you would like to create. Birth plans are generally discussed in your childbirth classes. Look in various childbirth books early on in your pregnancy and begin to educated yourself. A few favorites are, “The Birth Book” by Sears and Sears, MD, “The Complete Book for Pregnancy and Childbirth,” by Sheila Kitzinger and “New Active Birth, a Complete Guide to Natural Childbirth,” by Janet Balaskas. To find out about midwifery based practices in your area, call American College of Nurse Midwives, (ACNM,): 202-728-9860 (general number), 1-888-643-9433, (toll free locator number). Or contact Midwives Alliance of North America, (MANA): 1-888-923-6262.
Bring questions to your medical caregivers, be attentive how they respond. If you experience not being heard or rushed through prenatal visits, go over in your mind and with your partner why you don’t feel supported. If you do your work early on, talking further or switching medical caregivers will not be as problematic.
Over and over I have encouraged women to trust your highly sensitized instincts, do research and own this birth. This labor and birth will only happen once and it’s vital to be with people you feel safe, listened to and trust. I believe, the only way change will take place among the obstetrical practices is through the public. By asking for what you deserve, you educate and introduce the medical profession to another possibility.
Another alternative is a labor support doula. A ‘doula’ is a Greek word for ‘woman assistant.’ She meets with a couple and gathers information prentally. She’s on call before and after the due date, attending to the parents needs during early and later stages of labor and birth, following up with a post-natal visit after the birth. Doulas have statistically proven to lower cesarean sections by 50%, length of labor down 25%, oxytocin use, down 40%, pain medications (narcotics) down 30%, forceps down 30%, and epidurals down 60%. A labor doula is by no means to replace the partner of the mother. No one can replace the relationship or connection of a woman’s partner. The doula helps to relieve the pressure and enhance the experience.
Since 1993, when Doulas of North America, (DONA,) began a certification program there are now over 8,000 certified. For referrals call, 206-324-5440. Book referrals for becoming a doula: “The Birth Partner,” by Penny Simkin, PT, “Mothering The Mother,” by M. Klaus, MD , J. Kennel, MD and Phyllis Klaus, M.Ed., CSW. If someone would be interested in setting up a doula program read, “Doula Programs: How to Start and Run Private or Hospital-Based Programs with Success!,” by Paulina Perez and Deaun Thelen.
An aquatic analgesic alternative to medical pain medication or an epidural is water labor or water birth. As the east coast resource center for water birth, my organization, Birth Balance, has educated countless couples on this unique and growing approach. A shower is great during labor, yet, it can’t compare to submerging half to three quarters of your body in a tub of water. Advantages to water birth for the mother are: easier coping during dilatation of the cervix and the pushing stage, softening of the perennial tissues, bones, muscles so lacerations are minimal, ability to move in whatever position her body organically discovers, less interventions, faster labors and births. Advantages to the baby: a medium which softens the baby’s bones and tissues thus creating a softer birth experience, babies appear to be less traumatized, a drug free beginning and more immediate bonding with mother.
 A concern regarding water labor or birth is infection. When in the water, bacteria is diluted. Unless someone enters the water with an infection of some sort offering foreign bacteria, there wouldn’t be problems with the mothers infecting herself or the baby. A study in 1996 of 1385 women with prelabor rupture of the membranes after 34 weeks gestation concluded a tub bath did not increase the risk of maternal or neonatal infection after premature rupture of the membranes and prolonged latency. (1)
A concern regarding water labor or birth is infection. When in the water, bacteria is diluted. Unless someone enters the water with an infection of some sort offering foreign bacteria, there wouldn’t be problems with the mothers infecting herself or the baby. A study in 1996 of 1385 women with prelabor rupture of the membranes after 34 weeks gestation concluded a tub bath did not increase the risk of maternal or neonatal infection after premature rupture of the membranes and prolonged latency. (1)
Another randomized, controlled trial was with 785 women. The results were as follows: tub group required fewer pharmacological agents, fewer deliveries by forceps and vacuum, more likely to have intact perineum and an overall positive effect on analgesic requirements, instrumentation rates, condition of the perineum and personal satisfaction. (2)
Another concern people have is the drowning of the baby at birth. The baby is in a womb of water from conception and is born into an extended womb of water later. The baby receives oxygen from the umbilical cord which is attached to the placenta. As the baby is born, the placenta is detaching from the mother, thus the supply of oxygen becomes depleted and bringing the baby up to the surface as soon as possible is imperative. Another atmospheric pressure, such as air or gravity is what stimulates the babies chemoreceptors to take a breath. That is why, in water, the baby will not take a breath.
Water birth has been around for centuries. In the contemporary times the concept began in Russia in the 60’s,, spread to France, England in the 70’s and come to the United States in the 80’s. For further reading on the subject check out: (book and video) “Gentle Birth Choices,” by Barbara Harper, RN, “Water Birth, A Midwife’s Perspective,” by Susanna Napierala and “The Waterbirth Handbook, ” by Dr. Roger Lichy and Eileen Herzberg.
No matter what choices you make for this birth or future, each pregnancy, labor and birth will teach you what to do differently or the same the next time. Remember, everything is an opportunity for learning. Keep an open mind and heart and learn.
(1), (2): MIDIRS Midwifery Digest, (Mar 1997) 7:1.


 When I asked the father why he chose to attend the labor and birth of his partner, the responses were uplifting. “Why not?” said a new daddy, “It’s my child as well. To me it was a moment getting to know and get closer to my wife. I can assure you, it did. It took the relationship to another level. Relationships are a collection of experiences and it’s brought us closer together. Forget the candlelight dinners guys, you can’t compare it and it may happen only once or twice in your life. Don’t miss it.”
When I asked the father why he chose to attend the labor and birth of his partner, the responses were uplifting. “Why not?” said a new daddy, “It’s my child as well. To me it was a moment getting to know and get closer to my wife. I can assure you, it did. It took the relationship to another level. Relationships are a collection of experiences and it’s brought us closer together. Forget the candlelight dinners guys, you can’t compare it and it may happen only once or twice in your life. Don’t miss it.”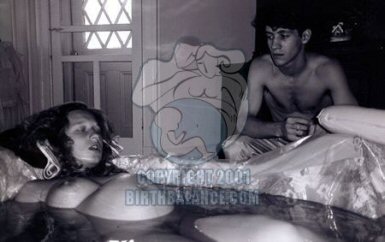

 in a nursing school and continued until she got sick and decided to become an independent midwife.
in a nursing school and continued until she got sick and decided to become an independent midwife. The labor and birth area, downstairs, contains an aqua blue oval tub, covered with a sterile plastic cover, weighted down by sterling sliver dolphin, moon and starburst clips, keeping the tub clean and available to use at any time. The tub is next to a cluttered desk, a bed that rotates up and down, colorful bean bags to sit or lean on, a short low birth chair, a geriatric stool to lean over with a hidden foam pad which Yamada quickly retrieves from under the bed. With a press of a button a heat a toilet is seated. With a press of a few more buttons a genital area is washed and dried automatically. Ah, the wonders of another country. Yamada believes in low light levels and keeps the overhead lights off and the decorative side wall lights on. Midwives utilize an underwater doppler stethoscope to check the babies heart tones. The house includes steep staircases, a modest kitchen, an additional room with a jacuzzi tub, areas for weighing, bathing and checking the jaundice levels of the babies.
The labor and birth area, downstairs, contains an aqua blue oval tub, covered with a sterile plastic cover, weighted down by sterling sliver dolphin, moon and starburst clips, keeping the tub clean and available to use at any time. The tub is next to a cluttered desk, a bed that rotates up and down, colorful bean bags to sit or lean on, a short low birth chair, a geriatric stool to lean over with a hidden foam pad which Yamada quickly retrieves from under the bed. With a press of a button a heat a toilet is seated. With a press of a few more buttons a genital area is washed and dried automatically. Ah, the wonders of another country. Yamada believes in low light levels and keeps the overhead lights off and the decorative side wall lights on. Midwives utilize an underwater doppler stethoscope to check the babies heart tones. The house includes steep staircases, a modest kitchen, an additional room with a jacuzzi tub, areas for weighing, bathing and checking the jaundice levels of the babies. washing the baby in the bath before they leave the House. Yamada teaches only the father how to bathe the baby, not the mother. This is a way to establish a special commitment from the father in his assistance and caregiving for the child. The bath is not given the first day of the birth, only the second day after. Every day Yamada checks the babies jaundice with a small, handheld portable machine.
washing the baby in the bath before they leave the House. Yamada teaches only the father how to bathe the baby, not the mother. This is a way to establish a special commitment from the father in his assistance and caregiving for the child. The bath is not given the first day of the birth, only the second day after. Every day Yamada checks the babies jaundice with a small, handheld portable machine. Yamada’s assistant and midwife in training, Ms. Megumi Tanaki was seven months pregnant when I did the interview. Tanaki’s background as a nurse for many years in a private hospital and University Medical Hospital left her feeling limited as a nurse. Tanaki shares, “When I worked as a shift nurse and the Hospital became bigger and bigger, I wasn’t able to manage what I wanted to do as a nurse because it is institutionalized and I had to work as a group organization.”
Yamada’s assistant and midwife in training, Ms. Megumi Tanaki was seven months pregnant when I did the interview. Tanaki’s background as a nurse for many years in a private hospital and University Medical Hospital left her feeling limited as a nurse. Tanaki shares, “When I worked as a shift nurse and the Hospital became bigger and bigger, I wasn’t able to manage what I wanted to do as a nurse because it is institutionalized and I had to work as a group organization.” babies, my physical balance is quite good. I believe my hormones become more balanced when I assist the births with the mothers and babies. I work in good circumstances so this is my happiness,” concludes Tanaki.
babies, my physical balance is quite good. I believe my hormones become more balanced when I assist the births with the mothers and babies. I work in good circumstances so this is my happiness,” concludes Tanaki.



 If you are fortunate enough to be invited into the OR in a hospital,
If you are fortunate enough to be invited into the OR in a hospital,



 ~
~ Of course, I am in favour of the abolition of electronic fetal monitoring but it would be far more uplifting if this was being done for some sort of health improvement and not just more ways to cover butt in court.
Of course, I am in favour of the abolition of electronic fetal monitoring but it would be far more uplifting if this was being done for some sort of health improvement and not just more ways to cover butt in court. One of the midwife “tricks” that we were taught was to ask the mother’s shoe size. If the mother wore size five or more shoes, the theory went that her pelvis would be ample. Well, 98 percent of women take over size five shoes so this was a good theory that gave me confidence in women’s bodies for a number of years. Then I had a client who came to me at eight months pregnant seeking a home waterbirth. She had, up till that time, been under the care of a hospital nurse-midwifery practise. She was Greek and loved doing gymnastics. Her eighteen-year-old body glowed with good health, and I felt lucky to have her in my practise until I asked the shoe size question. She took size two shoes. She had to buy her shoes in Chinatown to get them small enough—oh dear. I thought briefly of refreshing my rusting pelvimetry skills, but then I reconsidered. I would not lay this small pelvis trip on her. I would be vigilant at her birth and act if the birth seemed obstructed in an unusual way, but I would not make it a self-fulfilling prophecy. She gave birth to a seven-pound girl and only pushed about twelve times. She gave birth in a water tub sitting on the lap of her young lover and the scene reminded me of “Blue Lagoon” with Brooke Shields—it was so sexy. So that pelvis ended the shoe size theory forever.
One of the midwife “tricks” that we were taught was to ask the mother’s shoe size. If the mother wore size five or more shoes, the theory went that her pelvis would be ample. Well, 98 percent of women take over size five shoes so this was a good theory that gave me confidence in women’s bodies for a number of years. Then I had a client who came to me at eight months pregnant seeking a home waterbirth. She had, up till that time, been under the care of a hospital nurse-midwifery practise. She was Greek and loved doing gymnastics. Her eighteen-year-old body glowed with good health, and I felt lucky to have her in my practise until I asked the shoe size question. She took size two shoes. She had to buy her shoes in Chinatown to get them small enough—oh dear. I thought briefly of refreshing my rusting pelvimetry skills, but then I reconsidered. I would not lay this small pelvis trip on her. I would be vigilant at her birth and act if the birth seemed obstructed in an unusual way, but I would not make it a self-fulfilling prophecy. She gave birth to a seven-pound girl and only pushed about twelve times. She gave birth in a water tub sitting on the lap of her young lover and the scene reminded me of “Blue Lagoon” with Brooke Shields—it was so sexy. So that pelvis ended the shoe size theory forever.














