So why would one want to do anything with a placenta other than grow a baby in one and discard it after the birth? That’s a question I get far too often when I bring up the possibility of doing something with the placenta after the birth.
 Some people plant trees or bushes over it, other’s bury it in a garden to enrich the soil and celebrate the new life given to them. It is a dedication of the placenta back to the earth in honor of the child coming into their lives. A year later, a tree, flower, bush is planted in the same spot to allow the placenta to nourish it’s growth. The waiting of a year is to assure the growth or a new seedling because the nutrient rich placenta can potentially kill anything planted before a year. There are what reader Judy Pfeifer calls “birthing bushes” across the city: flowering yews, almond trees, lilies, camellias, raspberry canes and tomatoes. Roses are popular bushes to plant atop a child’s placenta – and they flourish, I’m told. Magnolias, not so.
Some people plant trees or bushes over it, other’s bury it in a garden to enrich the soil and celebrate the new life given to them. It is a dedication of the placenta back to the earth in honor of the child coming into their lives. A year later, a tree, flower, bush is planted in the same spot to allow the placenta to nourish it’s growth. The waiting of a year is to assure the growth or a new seedling because the nutrient rich placenta can potentially kill anything planted before a year. There are what reader Judy Pfeifer calls “birthing bushes” across the city: flowering yews, almond trees, lilies, camellias, raspberry canes and tomatoes. Roses are popular bushes to plant atop a child’s placenta – and they flourish, I’m told. Magnolias, not so.
Actor Matthew McConaughey brought this ritual into news when he announced he planned to plant the placenta of his son, Levi, in an orchard. If you are planning to plant the placenta, you can freeze it until you are ready to plant. After a year in the ground, the placenta breaks down in the soil and delivers nutrients that will produce a beautiful tree, bush or flower. You can even put together a ‘placenta planting party’ and turn the event into a big celebration honoring your child on their first birthday. A tender suggestion from Loreen Lee: “I think this calls for a garden burial, then above the spot a sandbox and playhouse with a little plaque, `Noah’s place – enter here.’” Jeanne Mott’s grandsons’ placentas are planted beneath trees that bear flowers and berries in spring, she writes, and a tree with heart-shaped leaves that turns rich shades of golden-orange for her October-born granddaughter. “(The children) all refer to the trees as `my tree,’ and it has become part of their personal identity in their yard, cementing their sense of place perhaps. Just a little thing, but rather sweet.”
 To make a placenta print, you take a piece of watercolor paper and lay the placenta on it, along with the cord attached. Let it dry and then choose paints to add color to the piece. Hang it in a boxed frame because the ‘ink’ is a blood born base and it protects the art as well as others being exposed to the material, or store the piece for safekeeping. I was at a birth recently for twins where they were NOT allowed to remove the placentas from the hospital, so I brought in 4 large pieces of art paper and when most of the staff had left the OR (operating room), the head nurse allowed me to make some placenta art for the parents to take home. They had a vaginal birth with the twins! This placenta print here is by Patience of Art of Patience. You may see her other work at: http://artofpatience.ourprairie.net
To make a placenta print, you take a piece of watercolor paper and lay the placenta on it, along with the cord attached. Let it dry and then choose paints to add color to the piece. Hang it in a boxed frame because the ‘ink’ is a blood born base and it protects the art as well as others being exposed to the material, or store the piece for safekeeping. I was at a birth recently for twins where they were NOT allowed to remove the placentas from the hospital, so I brought in 4 large pieces of art paper and when most of the staff had left the OR (operating room), the head nurse allowed me to make some placenta art for the parents to take home. They had a vaginal birth with the twins! This placenta print here is by Patience of Art of Patience. You may see her other work at: http://artofpatience.ourprairie.net
Still, placentophagy, eating a placenta cooked or not cooked, isn’t something recently dreamed up by crunchy granola types — it’s been going on in many parts of the world for centuries:
- In parts of Indonesia, the Czech Republic and Morocco, new mothers once believed eating the placenta guarantees future fertility.
- Once women in Hungary had tired of the whole child-bearing business, they believed that by burning the placenta and placing the ashes in their husband’s drink, he’d soon be shooting blanks.
The German word for placenta is Mutterkucken and the Dutch word for it is Moederkoek. Both words mean “mother-cake.”
 Among the Hmong culture of Southeast Asia, the word for placenta can be translated as “jacket,” as it’s considered an infant’s first and finest clothing. The Hmong bury the placenta outside. They believe that after death, the soul must retrace the journeys undertaken in life until it reaches the burial place of its placenta jacket.
Among the Hmong culture of Southeast Asia, the word for placenta can be translated as “jacket,” as it’s considered an infant’s first and finest clothing. The Hmong bury the placenta outside. They believe that after death, the soul must retrace the journeys undertaken in life until it reaches the burial place of its placenta jacket.
Buddhists liken the unfolding of the lotus petals to the unfolding of the divine within the human self. The closed bloom represents the heart with its infinite potential for enlightenment. The open blossom represents the enlightened self. Lotus jewelry is a cherished keepsake for the new mother after a lotus birth.
Among the Navajo Indians of the Southwest, it’s customary to bury a child’s placenta within the sacred Four Corners of the tribe’s reservation as a binder to ancestral land and people. New Zealand’s Maoris have the same tradition of burying the placenta within native soil. In their native language, the word for land and placenta are the same: whenua.
The indigenous Bolivian Aymara and Quecha people believe the placenta has its own spirit. It is to be washed and buried by the husband in a secret and shady place. If this ritual is not performed correctly, they believe, the mother or baby may become very sick or even die.
The Ibo of Nigeria and Ghana treat the placenta as the dead twin of the live child and give it full burial rites.
Filipina mothers are known to bury the placenta with books, in hopes of a smart child.
Other cultures place a symbol of their people with the placenta when burying it, as a kind of heritage insurance.
Gossip blogs have said Eva Longoria keeps her baby face by using EMK Placental Face Cream, an $85 product which uses placenta protein extract. Tribes in the Ural Mountains in Russia thought of the placenta as a caretaker for the child — and as such, it deserved a warm welcome. Along with carefully knitted clothes for the infant, they’d create a tiny shirt for the placenta. Some Maori women in New Zealand believe the afterbirth must be buried immediately, and that disposing it in any other way will harm the child.
One group of Siberian people believed when the baby laughed in its sleep, it was because the soul of the placenta had visited it. In parts of Norway, mothers would stab the placenta with a knife, believing it was a horrible monster that must be killed.
“It’s an organ. So, just like any organ meat, if it wasn’t kept well — if it wasn’t frozen or kept at a cool temperature — you have a danger of bacteria or something growing,” Schorn says. “But there’s nothing inherent about placenta that would make it more dangerous than any other meat.”
There are recipes for cooking placentas such as, placenta stew, placenta lasagna, power drinks and others. Some choose to eat the placenta raw. Consumption of uncooked human placenta carries risks associated with other human blood products. There is the risk of hepatitis B,C, and HIV infection. If you eat your own placenta, it does not carry these risks. There are many reasons for eating the placenta after a birth. It helps the womb to contract. Many animals eat their own placenta as a means to hide the scent from predators.
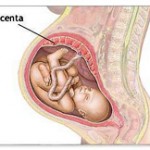
 The placenta is a living organ, filled with natural oxytocins, attached to the mother’s womb where it draws nourishment and oxygen from the mother and delivers it to the baby via the umbilical cord. The placenta joins the mother to the baby and the baby to the mother. It is truly the baby’s “life support” system during the pregnancy. It is about 1/6th of the baby’s weight. It acts as an endocrine gland, producing estrogen, progesterone and gonadotrophin. The womb and the placenta have a fine membrane separating them. Surprisingly, the blood of the mother and the baby do not mix.
The placenta is a living organ, filled with natural oxytocins, attached to the mother’s womb where it draws nourishment and oxygen from the mother and delivers it to the baby via the umbilical cord. The placenta joins the mother to the baby and the baby to the mother. It is truly the baby’s “life support” system during the pregnancy. It is about 1/6th of the baby’s weight. It acts as an endocrine gland, producing estrogen, progesterone and gonadotrophin. The womb and the placenta have a fine membrane separating them. Surprisingly, the blood of the mother and the baby do not mix.
Placentas have a life and mind of their own, connected energetically and physically to the mind of the baby and the mother. Sometimes the placentas register in the womb in an anterior or posterior, low lying (placenta previa) or high lying position. If the placenta is low-lying, near the cervix, there is an imagery exercise one can do to help “raise up the placenta” so a vaginal birth is possible. Placentas can also be attached too deeply into the womb wall, (placenta accrete) which might cause problems with the removal after the birth of the baby. Imagery can be helpful here as well.
Preparing the placenta for consumption by mothers is considered traditional among Vietnamese and Chinese people. The Chinese believe a nursing mother should boil the placenta, make a broth, then drink it to improve her milk. Traditional Chinese Medicine consider the placenta a powerful and sacred medicine full of life force, Qi. Chinese women thought a bite of dried placenta would speed up labor. They make medicinal capsules and/or herbal – homeopathic tinctures out of it. Some consider it cannibalism, others find it extremely helpful to ward off ‘baby blues’ experienced in about 80% of women in the first few days or weeks after the birth. Some situations become more severe and post partum depression, (PPD) may evolve. The placenta medicine has been known to; ward off both the blues and PPD, shorten the post bleeding time, restore lost hormones, nourish the blood, replenish depleted iron, reduce the overall recovery time from labor and birth for baby and mother after the birth, increase energy, boost the immune systems and enhance milk production. Placentophagy, or consumption of the placenta has been around for centuries.
The Science of Placenta Medicine (from www.placentabakery.com)
The known ingredients that give the placenta its healing properties are:
Gonadotrophin: the precursor to estrogen, progesterone and testosterone,
Prolactin: promotes lactation,
Oxytocin: for pain and bonding; produced during breastfeeding to facilitate bonding of mother and infant. In pharmaceutical form this is a very addictive drug because it promotes a feeling of connectedness with others,

Thyroid stimulating hormone: boosts energy and helps recovery from stressful events,
Cortisone: combats stress and unlocks energy stores,
Interferon: stimulates the immune system to protect against infections,
Prostaglandins: anti-inflammatory,
Hemoglobin: replenishes iron deficiency and anemia, a common postpartum condition,
Urokinase inhibiting factor and factor XIII: stops bleeding and enhances wound healing,
Gammaglobulin: immune booster that helps protect against postpartum infections.
So, as you can see, the placenta is full of feel-good hormones and healing chemicals,
Clinical Research: (from www.placentabakery.com)
“It has been shown that the feeding of desiccated placenta to women during the first eleven days after parturition causes an increase in the protein and lactose percent of the milk… All the mothers were receiving the same diet, and to the second set 0.6mg of desiccated placenta was fed three times a day throughout the period. Certain definite differences in the progress of growth of the two sets of infants are to be observed. It is evident that the recovery from the postnatal decline in weight is hastened by the consumption of milk produced under the influence of maternally ingested placenta.” McNeile, Lyle G. 1918. The American journal of obstetrics and diseases of women and children, 77. W.A. Townsend & Adams, original press: University of Michigan.
Powdered Placenta Hominis was used for 57 cases of insufficient lactation. Within 4 days, 48 women had markedly increased milk production, with the remainder following suit over the next three days.” Bensky/Gamble. 1997. Materia Medica, Eastland Press, 549.
“All patients were given desiccated placenta prepared as previously described (C.A. II, 2492) in doses of 10 grains in a capsule 3 times a day. Only those mothers were chosen for the study whose parturition was normal and only the weights of those infants were recorded whose soul source of nourishment was mothers milk. The growth of 177 infants was studied. The rate of growth is increased by the ingestion of placenta by the mother… the maternal ingestion of dried placenta tissue so stimulates the tissues of the infants feeding on the milk produced during this time, that unit weight is able to add on greater increments of matter, from day to day, than can unit weight of infants feeding on milk from mothers not ingesting this substance.” Hammett, Frederick. S. 1918. The Journal of Biological Chemistry, 36. American Society of Biological Chemists, Rockefeller Institute for Medical Research, original press: Harvard University.
“Giving…placenta to a new mother following birth has become standard protocol among a growing number of midwives in the United States. By nourishing the blood and fluids, endocrine glands and organs, Placenta will …reduce or stop postpartum bleeding, speed up recovery, boost energy and relieve postpartum blues.” Homes, Peter. 1993. Jade Remedies, Snow Lotus Press, 352.
This is the LONGEST umbilical cord I have seen in my 23 year career: 38.5 inches long. Normal is: 20ish”

Then, there’s the not-so-ceremonial use of it, the commercial use of “placenta extract” found in some cosmetics, such as facial cream sold in France. In 1994, Britain banned the practice of collecting placentas in hospitals from unsuspecting mothers, after it was learned that 360 tons of it were annually being bought and shipped by French pharmaceutical firms. They used it to make a protein, albumin, for burns and to make enzymes to treat rare genetic disorders. Did you know that many beauty products contain placenta? (Jodome Organic Placenta Soap)
Freezing the placenta is not suggested unless it is for a short period of time. (up to 3 months) If you do freeze your placenta, it is best to double zip-lock it in gallon sized bags with all the excess air squeezed out within an hour or so of the birth. Refrigeration for any ‘length’ of time will result in ‘spoiled meat’ and the placenta will not be viable. If you are having your baby in the hospital you must speak with your medical caregiver ahead of time, before the labor and birth about taking it home with you. Most hospitals have a protocol to bring your placenta to pathology, keep it for five or more days and then discard it. It will not be refridgerated and probably put in formaldihyde. You must not use the placenta at this point. Make special arrangements with the hospital staff to either release it right away or have it immediately frozen rather than refrigerated if they insist on keeping it for a period of time. Legally the placenta is your property. They may require you to sign forms upon admission regarding the after birth. You may just write, “I do not consent” on the form.
It must be in your birth plan at the time to delay cord clamping and cutting until the cord has totally stopped pulsing. Early cord clamping leaves the placenta engorged with blood and the baby is deprived of up to half of their blood volume and vital stem cells.
So what is the proper way to prepare an encapsulation of the placenta? Every website will explain it a little differently. It is best to encapsulate within 2-3 days after the birth. I find when I steam the placenta before I dry it, there are fewer pills than when I just rinse the placenta with cold water, cut it into thin slices and dehydrate it. The ‘energy’ put into the preparation will go into the capsules, so healing prayers, music and laughter is best when preparing the medicine. One can pay someone to do the procedure, which can take from 12-18 hours to do, or research and do it yourself. I can get between 130-250 pills per placenta. If I do not make an herbal tincture with part of the placenta and the sheath or sacs, I can get more pills. Contrary to what many people say, I actually DRY the amniotic sacs and pulverize with the rest of the placenta parts. I also add a bit of dried lemon grass, echinacea and garlic to help boost the immune system to the mother and the baby. Lemon grass treats problems with digestive systems and is useful for relieving muscle spasms. It also balances the nervous system and provides a gentle boost when exhausted. Echinacea stimulates the immune system and promotes T-cell activation. It helps white blood cells attack germs. Garlic is well known as the “wonder drug” for boosting the immune system. By adding a small amount of each of these herbs to the capsules, the color of the pills may change from a darkish black to a lighter brown.
After the capsules are made they suggest a postpartum course of 2 capsules at a time with white wine. The wine is suppose to disperse the energy of the placenta throughout the body. This dosage can be taken up to 3 times a day until the mother feels balanced out. The remaining medicine can be taken homeopathically for the times when one’s child may be undergoing separation anxiety, or first steps, weaning a baby, etc.
I also make herbal ‘tinctures’ with different parts of the placenta. I gestate the parts for 6 weeks in one hundred proof vodka in a glass jar. I put the name of the mother/baby and birthdate on the outside of the glass jar along with a particular word that will carry the vibration the mother would like to infuse in the medicine. Afterward I drain out the excess birth matter and give the client a quart jar of pure mother placenta tincture. She can put 10 drops in a small amount of water and drink it during the times of transition for her baby or herself after the capsules are finished. This becomes a remedy for her and the family for many years. If one chooses to break down the mixture 10, 20, 30 times, etc., in a mixture of 80% distilled water and 20% alcohol, they can have a homeopathic remedy for the rest of their lives!
Jeanine Parvati-Baker, a shamanistic midwife, taught me to cut the umbilical cord from the placenta, lay it out flat on a piece of wax paper overnight to dry and in the morning, roll the cord partially dried into a circle and let dry completely. Then I put the cord, a placenta capsule and some sage leaves into a small animal skin medicine bag I have made by a woman in Florida:
Charlotte Litton Bryant, charlo721@yahoo.com /Email. I encourage the parents to take the cord out each year, take a photo of it and observe how it changes as it dries every year. Jeanine would do a ‘reading’ each year for her children, just by looking at the changes in the cord.

There is a wonderful book called, “Placenta: The Gift of LIfe,” by Cornelia Enning. The book covers the rituals from around the world, and the historical use of placenta remedies used throughout the ages. There are recipes for ointments, essences and other remedies. This is a groundbreaking book and the only guide to using placenta currently on the market. To order go to: http://www.midwiferytoday.com/merchant2/merchant.mv? Store_Code=MT&Screen=PROD&Product_Code=MB01
 Another book about placenta medicine hot off the press: ”The Natural Healing Power of the Placenta” by midwife, Jenny West, LM, CPM. You may reach her to order a copy at: 505- 294-4359 or info@tubsntea.com or http://www.albuquerquehomebirth.com/contactJenny.htm
Another book about placenta medicine hot off the press: ”The Natural Healing Power of the Placenta” by midwife, Jenny West, LM, CPM. You may reach her to order a copy at: 505- 294-4359 or info@tubsntea.com or http://www.albuquerquehomebirth.com/contactJenny.htm
The placenta is a rich source of blood stem cells. ”Researchers at Children’s Hospital Boston and the Dana-Farber Cancer Institute report a surprising finding about embryonic development: the blood system begins to form not only in the embryo itself, but also in the placenta, the organ that nurtures the baby in utero.” To read more, go to: http://www.bio-medicine.org/biology-news/Placenta-Is-A-Rich-Source-Of-Blood-Stem-Cells-178-1/
Discarded placentas deliver researchers promising cells similar to embryonic stem cells. ”Routinely discarded as medical waste, placental tissue could feasibly provide an abundant source of cells with the same potential to treat diseases and regenerate tissues as their more controversial counterparts, embryonic stem cells, suggests a University of Pittsburgh study to be published in the journal Stem Cells and available now as an early online publication in Stem Cells Express.” To read more, go to:http://www.bio-medicine.org/biology-news/Discarded-placentas-deliver-researchers-promising-cells-similar-to-embryonic-stem-cells-1575-1/
This is an article put out by Search Time.com, partners with CNN on Friday, July 3, 2009. It’s entitled, “Afterbirth: It’s What’s For Dinner” By Joel Stein, an LA journalist. A professional placenta chef comes to Stein’s home to prepare his wife’s placenta into pills. There is a video included in the article: http://www.time.com/time/health/article/0,8599,1908194,00.html
A wonderful site to gather information and possibly order your own kit to encapsulate your placenta is: Placenta Benefits.info with Jodi Selander. There is an article in The Compleat Mother, Issue Number 87, 2008, $3, “Placenta For Postpartum Wellness,” by Jodi Selander, North Las Vegas, Nevada. To get a back copy of the issue: contact: Jodi McLaughlin, editor of The Compleat Mother at Jody@minot.com. If you would like to download the article from a URL, please go to:http://www.compleatmother.com/pdf/no.87-Fall’07.pdf. The download will take about 15 seconds with a fast connection and longer with a slower connection.
Check out the following video by Dr. Stuart Fischbein: Delayed Cord Clamping:
http://www.metacafe.com/watch/yt-WWCOzkSe85M/dr_stuart_fischbein_delayed_cord_clamping/
 British designer Alex Green had grander ambitions – he made a teddy bear out of one, which has caused a stir in England, where it’s still on display in art galleries. His point was to provoke thought about Western society’s disdain for an organ that sustains life. “I was trying to give the placenta a bit of PR,” he says. The name of the article about this is: “Placenta Teddy Bears, Meals Sier Debate, Revulsion. Inventive Uses for the Afterbirth Include Placenta Pill, Objects, Trees.” By Lauren Cox, ABC News Medical Unit, November 10, 2009:http://abcnews.go.com/Health/MindMoodNews/placenta-teddy-bear-turns-heads/Story?id=9043347&page=1
British designer Alex Green had grander ambitions – he made a teddy bear out of one, which has caused a stir in England, where it’s still on display in art galleries. His point was to provoke thought about Western society’s disdain for an organ that sustains life. “I was trying to give the placenta a bit of PR,” he says. The name of the article about this is: “Placenta Teddy Bears, Meals Sier Debate, Revulsion. Inventive Uses for the Afterbirth Include Placenta Pill, Objects, Trees.” By Lauren Cox, ABC News Medical Unit, November 10, 2009:http://abcnews.go.com/Health/MindMoodNews/placenta-teddy-bear-turns-heads/Story?id=9043347&page=1
MEDIA COVERAGE OF THE PLACENTA CONTROVERSY:
 Placenta pizza? Some new moms try old rituals, By Melissa Dahl MSNBChttp://www.msnbc.msn.com/id/22087790/
Placenta pizza? Some new moms try old rituals, By Melissa Dahl MSNBChttp://www.msnbc.msn.com/id/22087790/
 Ingesting the placenta: Is it healthy for new moms? By Steve Friess http://www.usatoday.com/news/health/2007-07-18-placenta-ingestion_N.htm
Ingesting the placenta: Is it healthy for new moms? By Steve Friess http://www.usatoday.com/news/health/2007-07-18-placenta-ingestion_N.htm
 Afterbirth: It’s What’s For Dinner, By Joel Stein Timehttp://www.time.com/time/health/article/0,8599,1908194,00.html
Afterbirth: It’s What’s For Dinner, By Joel Stein Timehttp://www.time.com/time/health/article/0,8599,1908194,00.html
New Moms Pop Placenta Pills, By Valerie Hauch, The Toronto Star, May 5, 2011 http://www.healthzone.ca/health/newsfeatures/article/985974–new-moms-pop-placenta-pills
Placenta Pill Makers Turn Afterbirth Into Nutritional Supplement For New Moms, By Michale McLaughlin, Huffington Post, Weird News, December 2, 2011 http://www.huffingtonpost.com/2011/07/20/placenta-pill-maker-nutritional-supplement_n_886420.html
Placenta Encapsulation – CTV National News, August 7, 2011 http://www.youtube.com/watch?v=KBfhXMKdREY&feature=youtu.be
The Rise of the Afterbirth Empire: Placenta Eating Gains Traction, Huffington Post, Video, Posted 08/23/11 and updated 10/24/11 http://www.huffingtonpost.com/2011/08/23/placenta-its-whats-for-dinner_n_934141.html?ir=Parents
Encapsulation Brooklyn – Placenta Eating in NYC, Brooklyn Mamas Netowrk, August 26, 2011 http://brooklyn.mamasnetwork.com/baby/encapsulating-brookyln-placenta-eating-in-nyc/
Placenta’s Hidden Health Benefits. Placenta Stew Anyone? By Mummy Buzz with The Ummy Mummy Club, August 24, 2011 http://www.yummymummyclub.ca/placentas-hidden-health-benefits
Placenta Pills To Beat Baby Blues? Women Say Consuming Placenta Helps in Postpartum Recovery, with ABC 7 News, TheDenverChannel.com, Ana Cabreara, Posted, August 2, 2011, updated August 5, 2011 http://www.thedenverchannel.com/news/28738890/detail.html
Hospitals May Ban This… Find Out Why Every Woman Really Needs And Is Entitled To Her Placenta After Birthing, Health and Fitness Magazine, August 2011 Edition.http://issuu.com/healthfitness.us/docs/h_fm_august_2011_lr/26
Would You Eat Your Placenta? Anderson Cooper, Wednesday, September 21, 2011 http://www.andersoncooper.com/2011/09/21/placenta/#c2366
Placenta Pill For Baby Blues, CTV News Calgary, October 25, 2011, http://calgary.ctv.ca/servlet/an/local/CTVNews/20111025/CGY_placenta_encapsulation_111025/20111025/?hub=CalgaryHome
The concept of a many-branched tree illustrates the idea that all life on earth is related to science, religion, philosophy, mythology and other areas. A tree of life is a mystical concept alluding to the interconnectedness of all life, a metaphor for common descent in the evolutionary sense and a motif in world theologies, mythologies and philosophies.
The tree of life is a powerful, life affirming symbol in almost every culture. With the branches reaching out towards the sky, roots embedded deeply in the earth, it dwells in three worlds: heaven, earth and underworld. It unites above and below. It symbolizes wholesome truth, stability and nobleness. When you are in need of stability and strength, imagine the tree of life.
Nature knows how without even thinking about it. From ‘mother’s milk’ to the ‘tree of life,’ both nourishing the baby inside and out. Can we ever marvel enough at it’s wonders and perfect design?
Disclaimer
The information on this page has not been evaluated by the Food and Drug Administration. The services I offer are not clinical, pharmaceutical, or intended to diagnose or treat any condition. Families who choose to utilize the services on this page take full responsibility for researching and using the remedies.




 If you are fortunate enough to be invited into the OR in a hospital,
If you are fortunate enough to be invited into the OR in a hospital,




 To make a placenta print, you take a piece of watercolor paper and lay the placenta on it, along with the cord attached. Let it dry and then choose paints to add color to the piece. Hang it in a boxed frame because the ‘ink’ is a blood born base and it protects the art as well as others being exposed to the material, or store the piece for safekeeping. I was at a birth recently for twins where they were NOT allowed to remove the placentas from the hospital, so I brought in 4 large pieces of art paper and when most of the staff had left the OR (operating room), the head nurse allowed me to make some placenta art for the parents to take home. They had a vaginal birth with the twins! This placenta print here is by Patience of Art of Patience. You may see her other work at:
To make a placenta print, you take a piece of watercolor paper and lay the placenta on it, along with the cord attached. Let it dry and then choose paints to add color to the piece. Hang it in a boxed frame because the ‘ink’ is a blood born base and it protects the art as well as others being exposed to the material, or store the piece for safekeeping. I was at a birth recently for twins where they were NOT allowed to remove the placentas from the hospital, so I brought in 4 large pieces of art paper and when most of the staff had left the OR (operating room), the head nurse allowed me to make some placenta art for the parents to take home. They had a vaginal birth with the twins! This placenta print here is by Patience of Art of Patience. You may see her other work at: 















 Placenta pizza? Some new moms try old rituals, By Melissa Dahl
Placenta pizza? Some new moms try old rituals, By Melissa Dahl 

 The argument for delayed cord clamping is often used as a springboard for those who believe in lotusbirthing, a more extreme version of delayed cord clamping.
The argument for delayed cord clamping is often used as a springboard for those who believe in lotusbirthing, a more extreme version of delayed cord clamping.








